Montreal mother opens up about her pregnancy complications due to pre-eclampsia
Posted July 31, 2024 8:24 pm.
Last Updated July 31, 2024 11:12 pm.
Nearly four months after she was born, baby Amalia Eva is still being cared for in the neonatal intensive care unit at Montreal’s Jewish General Hospital.
Her mother Tina Balais gave birth to her by emergency C-section on April 9th – she was born prematurely at 24 weeks, weighing only 510 grams.
“I was, like, surprised. Like, she made it, you know? She’s alive,” said Balais.

Balais had pre-eclampsia, a blood pressure condition that develops during pregnancy – restricting Amalia Eva’s ability to grow. It also put both mom and baby’s lives at risk.
“I couldn’t believe it, honestly. I couldn’t believe it. She was so tiny—really, really tiny, the size of like my hands. I was like, ‘What is that?’ She looked like a little monkey,” said Balais
Balais – overwhelmed – when she found out about her pregnancy complications.
“At the time, I just was really, really scared because I didn’t know what was happening. I didn’t know what they were going to do—were they going to deliver the baby that second, that night? I was really sick,” said Balais.
After Amalia was born, the challenges didn’t end. Care for premature babies like her often involves obstacles.
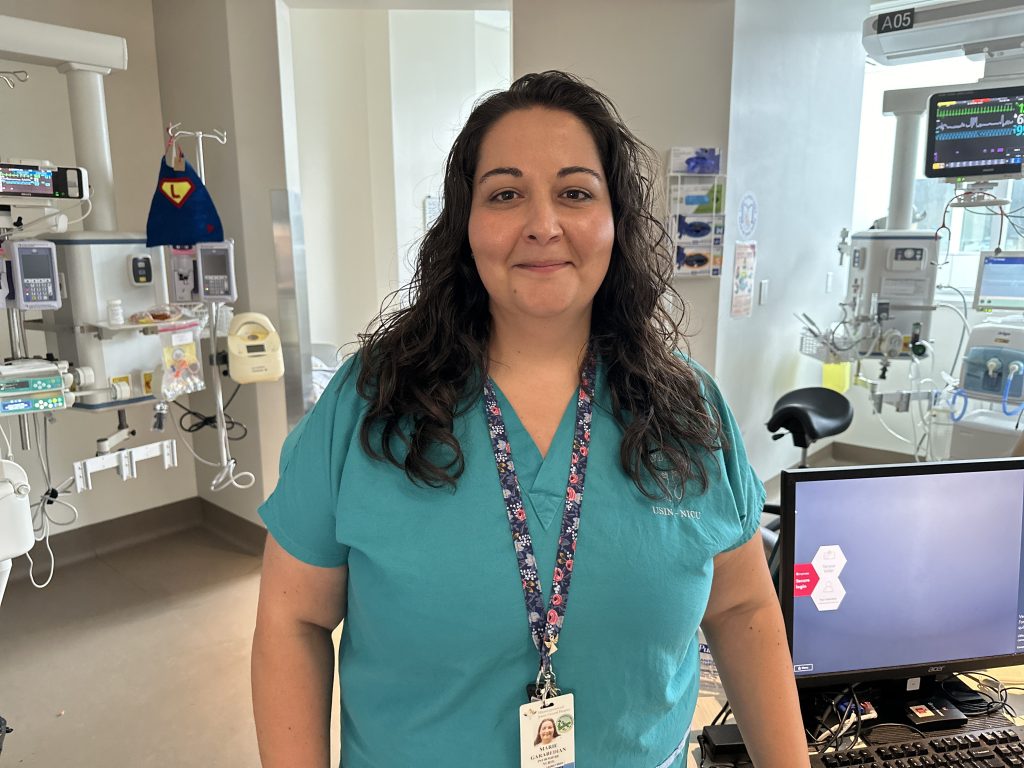
“The most common challenges are the multi-system complications that they have, including neurovascular, respiratory, developmental, cardiovascular, and endocrine. So it’s really about managing all the systems at once,” said Marie Garabedian, a clinical activity specialist for the NICU.
To help with respiratory issues, technology, like mechanical ventilators are used.
“The machine helps with the baby’s breathing. Sometimes it does all the breathing, or sometimes just a part of the breathing, in order to help them get over the phase where they need the help. Eventually, the baby is able to breathe more on their own, and we are able to reduce the amount of support,” said Lajos Kovacs, Chief of Neonatology and Pediatrics at the Jewish General Hospital.

“Also, of course, incubators in order to maintain the body temperature. Babies cannot do that in the ambient environment so they need high-tech incubators in order to regulate their body during the first several weeks of their hospital stay. Eventually when they’re a little bit bigger, we are able to stop the incubator and put them into a regular crib or skin-to-skin against the parents chest, which helps maintain their body temperature.”
Parents also play an important role in their child’s journey.
“The most important thing really including the parents. They are part of the multidisciplinary team; they are not just visitors,” said Garabedian.
Amalia’s growth is on track – and she now weighs 3-thousand and 65 grams – or 6 pounds and 12 ounces.
“It’s very rewarding to see an extremely premature baby like Amalia thrive, and progress, and develop, and go home, eventually, like Amalia will, is very rewarding.
Balais now sharing a message – to help others that may experience the same complications she did.
“If you’re pregnant and you’re feeling like there something is wrong, and even if the doctor is telling you it’s okay, but you know something is wrong, go to the emergency. Go to the emergency, tell them what you’re feeling— it could save your life. It could literally save your life,” said Balais.



