Breast cancer: knowing the symptoms, self-care after diagnosis and a ‘new era of blood tests’
Posted October 20, 2024 2:11 pm.
Last Updated October 20, 2024 7:42 pm.
One in eight Canadians will be diagnosed with breast cancer in their lifetime, and 22 Quebecers are diagnosed with breast cancer daily, according to the Quebec Breast Cancer Foundation (QBCF). The disease is on the rise in people in their 20s, 30s and 40s, according to a study from the University of Ottawa.
Montrealer Anna Capobianco-Skipworth was 41 when she was first diagnosed with breast cancer and has had 13 surgeries since. She prefers to be called a “breast cancer fighter.”
“I think laughter is really the best medicine,” she said.

“Being positive helps us get through it… [but you can’t] say that all of the women who died from breast cancer […] weren’t positive enough. We can’t have that kind of responsibility on our shoulders… You think I’m not anxious? You think I don’t make stories up in my head of what could happen? You don’t think I’m doing Dr. Google and seeing the worst? I am too.”
Anna Capobianco-Skipworth, Breast cancer fighter
Capobianco-Skipworth, who has been with the QBCF since 2001, picks up the phone to lend a supportive ear to her fellow breast cancer fighters whenever she can.
President and CEO of the QBCF, Karine-Iseult Ippersiel, agrees that a cancer diagnosis “brings anxiety.”
“It doesn’t matter what cancer you have, and there are many levels. The wait to find out if you have cancer is extremely heavy. We talk a lot about mental health and wellbeing in society. That’s something very heavy to carry for every person that is going through the process.”

Signs and symptoms
The recommended screening starts at 50, per the Canadian Task Force on Preventive Health Care’s guidelines. Yet 20 per cent of breast cancer cases are in people under 50 and early detection is the key factor in the five-year survival rate of almost 90 per cent.
Quebec Health Minister Christian Dubé recently mandated the Institut National d’Excellence en Santé et en Services Sociaux (INESSS) to evaluate the potential expansion of breast cancer screening starting at age 40.
“Everyone’s at risk for breast cancer,” said Ippersiel. “For example, a trans man will take hormones. So it increases the risk of breast cancer.
“Whether you’re gay, you’re trans, whether you’re Black, everyone has risk factors. We know that the Black community is more prone to triple-negative and the BRCA genes, and the risk starts a bit earlier. But there’s still not enough data, especially in Canada, for us to be able to have reliable data inflect on a screening program.”
Paying attention to the signs and symptoms is part of the Quebec Breast Cancer Foundation’s mission, which is a non-profit funded entirely by donations.
“Yes, it’s a bump, but there are many more,” said Ipperseil. “It could your breast that changes shape or drops [or] it could be one day your breast is heating, like it’s burning.
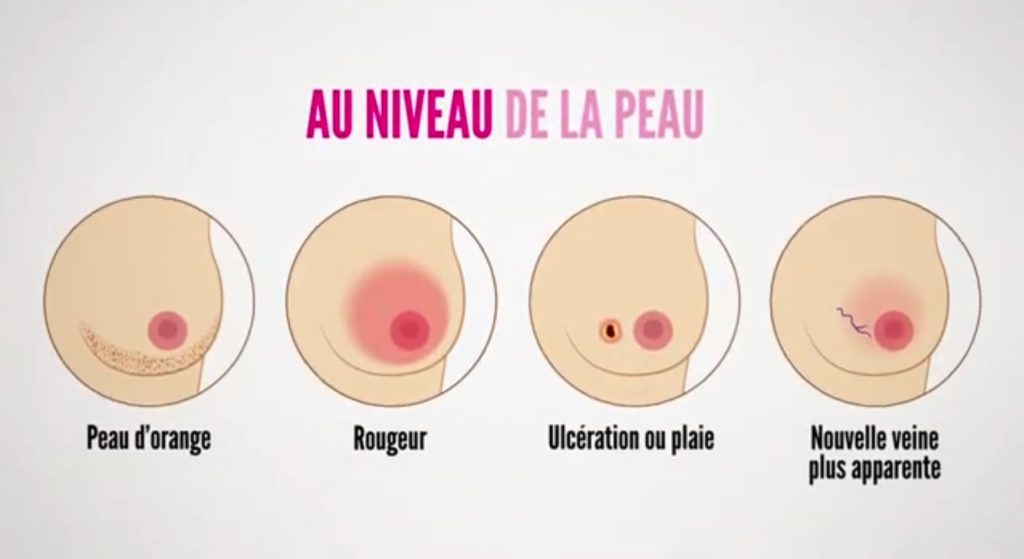

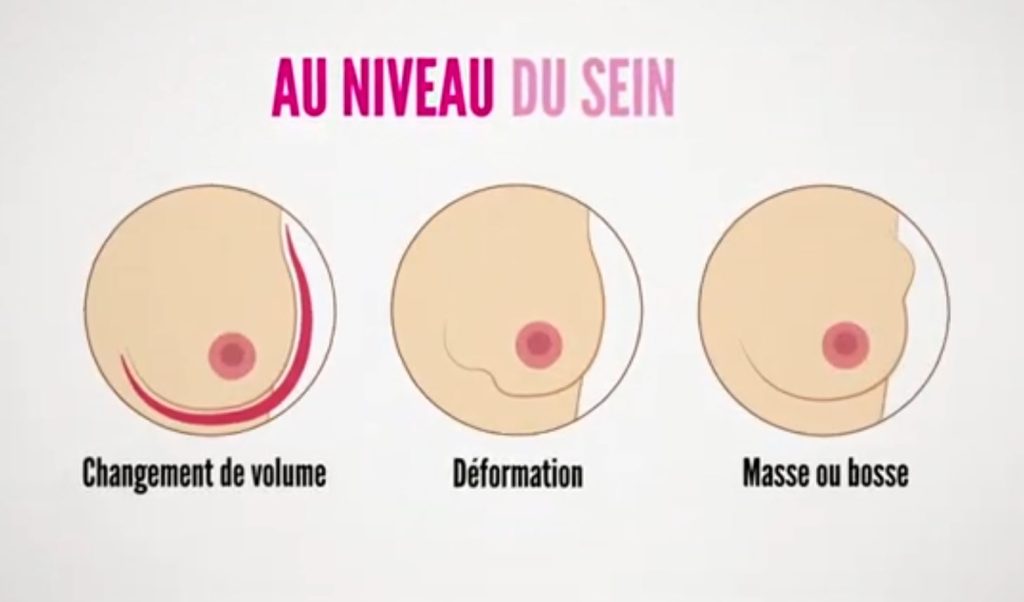
“There are all kinds of signs and symptoms and what we like to say, [it’s no longer just] the palpation test… If you see something that changes, whether it’s under the armpit or on your breast, just be quick to react. It’s always safer to go investigate than to wake up too late and then you have a stage four breast cancer.”
‘A new era of blood tests’ doctor says
Dr. Mark Basik’s research has focused on detecting early signs of tumours in the blood at the Cancer Genomics and Translational Research lab at the Jewish General Hospital in Montreal.
“That allows us to find it, like a needle in the haystack, literally, in the blood,” said the professor of surgical oncology at McGill University and a breast surgeon at the Jewish General Hospital.

“I think we’re ushering in a new era where the way blood tests […] will allow us to really get a much better picture of whether the cancer has spread, whether our treatment has worked, and even early on, whether it will work.”
For now though, mammography is still the most common test and detection for breast cancer, according to Basik.
“Mammography has improved in its quality. We have what’s called 3D mammography or tomosynthesis. So it’s better than it used to be 10, 20 years ago.”
Basik also explained that the biggest risk factor was family history. “For instance, in my family, my mother had breast cancer at the age of 50, so I would suggest that my sister start testing at 40.”
Knowing when to ask for help
Capobianco-Skipworth credits her husband for teaching her that it’s okay to laugh, and uses her fight with cancer as fodder for her stand up. Not long after her latest surgery, they hit the dance floor to celebrate the QBCF’s 30th anniversary.
“And if I was going to give a message to any woman who has been diagnosed, tell them you can cry, you can scream, you can be upset, you can be angry, you can do all of the emotions… and I even encourage it,” said Capobianco-Skipworth.
“Get it out, but then you need to know when it’s time to raise your hand and say, ‘help me up from the corner because I’ve been crying.'”











